"Interprofessional collaboration requires that responsibilities are clarified."
Jan. 2017Prevention in healthcare
Interprofessional collaboration. Interprofessional collaboration will play an increasingly important role in healthcare and prevention. Claudia Galli, President of the Swiss Federation of Professional Healthcare Organisations (SVBG), has agreed to outline the views of the healthcare professions in her responses to our questions.
Why has it taken so long to apply this approach in the healthcare system? What are the current obstacles?
Interprofessionality is an increasingly important trend and one that is worth following. Demographic changes, such as the increase in chronic diseases and an aging population together with an acute shortage of skilled staff, are forcing the healthcare sector to consider new models of cooperation and division of labour. The Swiss government's 'Health2020' strategy and all the associated national strategies include elements of coordinated care, and thus increase the significance of the interprofessional approach.
Of course, the previous debate on managed care also made us think increasingly in terms of networks. In fact this had a strong interdisciplinary focus from the start, in the form of cooperation between various specialists in the same profession. So the initial developments in the outpatient sector were basically physician networks. 'Interprofessionality' has only become important in recent years. It involves several professionals with different areas of expertise collaborating with one another as well as with patients, their relatives and the local network.1
Interprofessional collaboration is particularly important in challenging situations where a single profession doesn't have all the expertise necessary to satisfy complex requirements. But it involves more than just recruiting additional experts to treat the same patient. Different professional cultures come together in a team that believes in the importance of communicating with one another and achieving common goals. This means that each team member needs to reflect on his concept of himself as a professional, to re-examine existing hierarchical structures, to familiarise himself with the skills of other team members, and to act in the best interests of the patient. It goes without saying that this takes time.
Apart from any mental barriers, lack of funding is the greatest problem: as yet, no funding is available for coordination, communication, or the development of a new form of collaboration – particularly in the outpatient sector of healthcare. Another issue that makes it difficult to introduce interprofessionality into the healthcare system is the marked segmentation of training. Although there are interprofessional modules in the universities of applied sciences and individual training projects that involve the medical schools, where case-oriented ('problem-based') learning is increasingly common, there are still strong divisions between higher vocational schools, universities of applied sciences, and other universities. Firm establishment of interprofessionality as part of the professional identity of all health professionals would be a significant improvement. The Health Professions Act recently established this concept as part of the expertise required of health professionals graduating from universities of applied science.
Interprofessionality also means that more people are working for the patient's benefit. Doesn't this mean that costs will rise, or even that the patient's health could be jeopardised?
I can understand the concern that "too many cooks spoil the broth". But costs and error rates increase just when coordination is not part of the normal routine. Interprofessional collaboration requires that responsibilities are clarified, that communication between the relevant professionals is effective, and that they apply and coordinate their skills for the patient's benefit. At the outset, this requires the investment of time and money. But the initial effort is worthwhile and all parties gain: quality and continuity of care are increased, collaboration is coordinated, the people who are involved are more satisfied and cost control is increased.2
What should one be aware of when working in interprofessional teams?
The following central factors are becoming increasingly clear: the setting must support interprofessional collaboration, which must be initiated and promoted by senior management; time to put it in place must be available; responsibilities must be allocated and explained, and clear leadership is required, which respects the various cultures of the different professional groups while building a joint culture of collaboration. Last but not least, effective, transparent and respectful communication is a key factor for success.3
Are there areas in health care where this approach works particularly well?
In rehabilitation and palliative care it is particularly important to determine the right expert for each task, because of the complexity of the patient’s situation. For example, this means that nursing staff, social workers, physiotherapists, occupational therapists, pastoral counsellors and the medical team work more often in a partnership of equals. We can also take a lesson from the medico-social centres in western Switzerland, whose teams (unlike those of many home care organizations in eastern Switzerland) are often multi-professional and make an interprofessional decision on who will lead the team on a case-by-case basis.
What do you think is the ideal way to apply interprofessional collaboration in the early diagnosis of dementia, mental illness or other non-communicable diseases?
The Interprofessionality Platform mediates collaboration among a variety of healthcare professionals, and has developed criteria for the assessment of interprofessional projects: for example, all participating professional groups and the patients must be involved right from the start.
In an ideal world, decisions on the implementation of prevention guidelines or standards would be made jointly by stakeholders such as counselling centres, health associations, primary healthcare providers, home care organisations and patients. The following questions would need to be answered: Where can patients, their relatives or employers find help or advice when they notice early signs of mental illness or other non-communicable diseases in someone? Under which circumstances should healthcare providers inform others about a problem they have noticed, and to whom? How can one guarantee privacy for this information? When should healthcare professionals meet for discussions? Who should take the leadership role, or is this decided on a case-by-case basis? Which measures should be suggested to the patient, and by whom? Ideally, interprofessional networks function across borders, such as those between outpatient and inpatient entities or between prevention and healthcare.
How does interprofessional collaboration support prevention in healthcare?
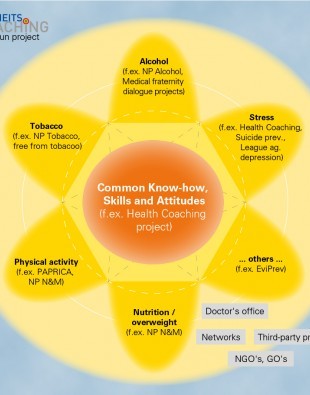
The perspectives and expertise available in the team have a synergistic effect when health professionals from different areas collaborate with one another. Prevention of non-communicable diseases is ineffective if only individual aspects are considered. As the NCD strategy shows, effective prevention needs an overall view of the patient’s situation. An interprofessional team makes this possible.
Personal details
Claudia Galli is President of the Swiss Federation of Professional Healthcare Organisations (SVBG) and has directed the European MSc programme in Occupational Therapy at the Zurich University of Applied Sciences (ZHAW) since 2012. She completed her training as an occupational therapist in 1991, and obtained a degree in psychology from the University of Zurich in 2002. As president of the SVBG she represents the interests of the health professions in various committees.
1 World Health Organisation (2010). Framework for action on interprofessional education and collaborative practice. Geneva, Switzerland: WHO.
2 World Health Profession Alliance (2013). WHPA Statement on Interprofessional Collaborative Practice (2013). Ferney Voltaire, France: WHPA.
3 See the meetings "How does interprofessionality succeed" which the Swiss Academy of Medical Sciences (SAMS) held in cooperation with the Interprofessionality Platform and other healthcare organisations in 2016 www.samw.ch/de/Projekte/Interprofessionalitaet/Tagungen-Interprofessionalitaet.html